The Tarnopol Triplets
Original due date - March 21, 2004
Anticipated due date - January ??, 2004
Bed rest date - October 1, 2003
Birthdate - January 20, 2004
What is Preeclampisa?
Preeclampsia is a disorder that occurs only during pregnancy and the postpartum period and affects both the mother and the unborn baby. Affecting at least 5-8% of all pregnancies, it is a rapidly progressive condition characterized by high blood pressure and the presence of protein in the urine. Swelling, sudden weight gain, headaches and changes in vision are important symptoms; however, some women with rapidly advancing disease report few symptoms.
What is Dexamethasone?
Dexamethasone is a synthetic corticosteroid used to promote fetal lung maturation in the third trimester, and is also found in some topical preparations.
What is an Gestational Diabetes?
Gestational diabetes is a type of diabetes that starts during pregnancy. If you have diabetes, your body isn't able to use the sugar (glucose) in your blood as well as it should, so the level of sugar in your blood becomes higher than normal.
Gestational diabetes affects about 4% of all pregnant women. It usually begins in the fifth or sixth month of pregnancy (between the 24th and 28th weeks), but in our case, 17 weeks. Most often, gestational diabetes goes away after the baby is born.
How can gestational diabetes affect me and my baby?
High sugar levels in your blood can be unhealthy for both you and your baby. If the diabetes isn't treated, your baby may be more likely to have problems at birth. For example, your baby may have a low blood sugar level or jaundice, or your baby may weigh much more than is normal. Gestational diabetes can also affect the mothers health. For instance, if your baby is very large, you may have a more difficult delivery or need a cesarean section.
What can I do if I have gestational diabetes?
You will need to follow a diet suggested by your doctor, exercise regularly and have blood tests to check your blood sugar level. You may also need to take medicine to control your blood sugar level.
What changes should I make in my diet?
Your doctor may ask you to change some of the foods you eat. You may be asked to see a registered dietitian to help you plan your meals. You should avoid eating foods that contain a lot of simple sugar, such as cake, cookies, candy or ice cream. Instead, eat foods that contain natural sugars, like fruits.
If you get hungry between meals, eat foods that are healthy for you, such as raisins, carrot sticks, or a piece of fruit. Complex sugars, which are found in foods like pasta, breads, rice, potatoes and fruit, are good for both you and your baby.
It's also important to eat well-balanced meals. You may need to eat less at each meal, depending on how much weight you gain during your pregnancy. Your doctor or dietitian will talk to you about this.
Why is exercise important?
Your doctor will suggest that you exercise regularly at a level that is safe for you and the baby. Exercise will help keep your blood sugar level normal, and it can also make you feel better. Walking is usually the easiest type of exercise when you are pregnant, but swimming or other exercises you enjoy work just as well.
You do need to be careful about how you exercise. Don't exercise too hard or get too hot while you are exercising. Depending on your age, your pulse shouldn't go higher than 140 to 160 beats per minute during exercise. If you become dizzy, or have back pain or other pain while exercising, stop exercising immediately, and call your doctor. If you have uterine contractions (labor pains, like stomach cramps) or vaginal bleeding, or your water breaks, call your doctor right away.
What tests will I need to have during my pregnancy?
Your doctor will ask you to have regular blood tests to check your blood sugar level. These tests will let your doctor know if your diet and exercise are keeping your blood sugar level normal. A normal blood sugar level is less than 105 mg per dL when you haven't eaten for a number of hours before the test (fasting) and less than 120 mg per dL 2 hours after a meal. If your blood sugar level is regularly higher than these levels, your doctor may ask you to begin taking a medicine called insulin to help lower it. You may be asked to see a specialist if you have to start taking insulin.
What happens after my baby is born?
You may not need to have blood tests to check your blood sugar while you're in the hospital after your baby is born. However, it may be several weeks after your baby's birth before your gestational diabetes goes away. To make sure it has gone away, your doctor will ask you to have a special blood test one or two months after you have your baby.
Even if the gestational diabetes goes away after the baby's birth, it makes you have a higher risk for diabetes in your next pregnancy and later in life. That is why it is important that you continue to exercise, watch your weight and eat a healthy diet. If you do these things, you may not get diabetes when you're older.
What is an Amniocentesis?
Amniocentesis is the removal of a small amount of amniotic fluid from the sac around the baby. The fluid contains cells which come from the baby and the placenta. This test is usually performed at 16 weeks in pregnancy.
After the skin is cleaned with antiseptic, a fine needle is inserted under ultrasound guidance through the mothers' abdomen into a pool of amniotic fluid. A small amount of the fluid is withdrawn and the needle removed. Most women find the procedure painless, although some women feel discomfort. After the procedure it is advisable to rest for the remainder of the day.
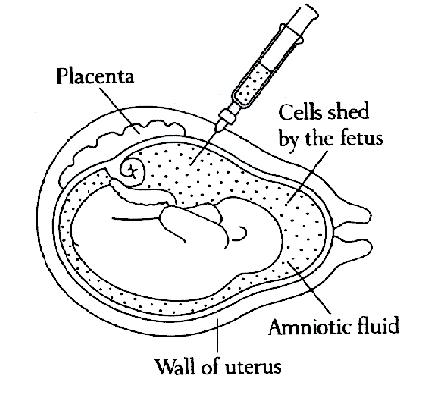
The amniotic fluid is sent to a lab for testing. A chromosome result will take 2-3 weeks. A biochemical result or direct genetic (DNA) test may take longer. The chromosome test establishes the sex of the baby and if you want to know this information you must ask the person giving you the results.
Amniocentesis carries a small risk of causing miscarriage. The average risk is 1 in 200 (half a percent). For 2 sacks, it is 1 in 100. Amnio may be offered to diagnose a number of birth defects in pregnancy. These include:
- Chromosome abnormalities e.g. Down Syndrome;
- Developmental problems e.g. Spina Bifida;
- Inherited disorders e.g. Cystic Fibrosis.
Why Would We Need The Test?
- Women over 35 have an increased risk of having a baby with a chromosomal problem;
- If there is a family history of chromosome problems and investigation shows that a prenatal test is appropriate;
- If there is a known disorder in the family which can be passed on to our baby e.g. Cystic Fibrosis, Muscular Dystrophy;
- If unexpected problems are detected on routine scan in early pregnancy.
What is Cervical Cerclage?
Cervical cerclage is a surgical procedure used to keep the cervix closed during pregnancy. The cervix is the lowest part of the uterus and extends into the vagina. During normal pregnancy it remains closed until the third trimester.
When is it used?
Cervical cerclage is used to prevent a miscarriage or premature delivery if you have an incompetent cervix. An incompetent cervix is a cervix that opens without labor too early in a pregnancy. Stitching around the cervix helps keep it closed as the babies grow.
If you have a history of second-trimester miscarriages, a cerclage may be done at the beginning of your second trimester. Otherwise it may be done at the time your Doctor finds that your cervix is opening too early. An alternative treatment for an incompetent cervix is bedrest that may last for several months.
How do I prepare for the procedure?
Follow instructions provided by your doctor. If you are to receive a general anesthetic, eat a light meal such as soup or salad the night before the procedure. Do not eat or drink anything after midnight before the procedure. Do not even drink coffee, tea, or water.
What happens during the procedure?
You will be given a general, spinal, or epidural anesthetic. Your doctor will then stitch a band of strong thread around your cervix. He or she will tighten the thread to hold the cervix firmly closed.
What happens after the procedure?
You may stay in the hospital for several hours or overnight so that you can be monitored for premature contractions or labor. Your doctor may give you medicine to reduce the chance that the procedure will start premature labor. Ask your doctor when you can have sexual intercourse again.
How long is the cerclage thread left in?
The thread is generally removed at the 37th week of pregnancy. If you have contractions or your bag of water breaks while the thread is still in, call your Dcotor right away.
What are the benefits of this procedure?
Cervical cerclage prevents miscarriage or premature delivery caused by cervical incompetence. The procedure is successful in 85% to 90% of cases.
What are the risks?
There are some risks associated with general anesthesia. If you are to have general anesthesia, discuss these risks with your doctor. This procedure is commonly done with a spinal anesthetic. The procedure may cause premature labor. The cervix may become infected. An infection may cause fever, chills, cramping, or a bad-smelling vaginal discharge. If you go into labor with the stitching in your cervix, your contractions may tear open your cervix. It is important that the stitching be removed before or during early labor. It is usually taken out without anesthesia. All of these complications rarely occur.
What are Monoamniotic Twins?
Monoamniotic twins, same sack twins, no dividing membrane. These are just a couple of the terms that are used to describe a rare condition that happens in just one percent (1%) of all identical twin pregnancies. It is a very difficult pregnancy complication, because the two babies are in the same amniotic sack with nothing keeping them from getting their umbilical cords tangled and knotted up.
I'll bet you were thinking that this happened in all identical twin pregnancies. The truth is that even an identical twin pregnancy usually has an amniotic sack for each baby. Only 1 out of 100 identical twin pregnancies end up with both babies in the same amniotic sack.
It happens due to the timing of the split. After the sperm and egg unite, they start dividing to make more cells. For identical twins, at some point, the clump of cells divides into two. The later that split happens, the more the babies have in common. From about 0 to 4 days, the split results in two babies, in their own amniotic sacks, and each has its own placenta, although the placentas may fuse together later. From 4 to 8 days, the babies generally share a placenta, a chorionic sack (the outer sack), and only have a thin dividing membrane that separates their amniotic sacks. From 8 to 12 days, the babies share an amniotic sack. After 12 days, conjoined twins are the usual result.
A Perinatologist, or Maternal-Fetal Medicine specialist, usually manages a monoamniotic pregnancy. These doctors specialize in high-risk obstetrics. However, the monoamniotic pregnancy is so rare (1 out of 25,000 pregnancies) than even a well-seasoned specialist may only see a 10 or 15 of these pregnancies in his or her entire career. The rarity of the condition also makes it hard to study in a traditional scientific/medical sense.